Our Work
Cord Blood Collection
Although some patients have family members who can donate stem cells, nearly 75% of patients will not find a matching donor in their family. Cord blood donation can give more patients hope by finding a suitable donor.
Cord Blood Unit is the nucleated cells including stem and hematopoietic progenitor cells
harvested from placental and umbilical cord blood vessels from placenta after the infant has been delivered and separated from the umbilical cord.
The cord blood is collected only with the mother's signed consent.
Collecting of the cord blood poses no health risk either to the mother or to the infant donor.
No collection is made if there are any complications during delivery.
To collect the cord blood remaining in the umbilical vein and placenta, the cord blood collector uses a sterile blood collection bag set with attached needle and punctures the cleaned surface of the cord with the needle to enter the umbilical vein. The cord drains through the tubing into the bag by gravity.
Cord blood can be donated only if the mother and infant are eligible.
Cord blood cannot be collected:
1. When the mother had an infectious disease during pregnancy that could have been transmitted to the infant before or during birth.
2. There is a family history of genetic disease that might be present in the baby.
3. The pregnancy was the result of an egg or sperm donation.
4. The infant has one of several genetic or inherited diseases.
Cord Blood Processing
Processing involves a series of steps to remove excess red blood cells (RBC's) and plasma and bring each collection down to a uniform single unit volume of 20 ml.
The processing is performed by an automated Sepax system. This system allows the fast, automated and reproducible processing of blood component in a functionally-closed and sterile environment.
The uniform single unit volume contains nearly all of the mononuclear blood cells present in the original collection, including the hematopoietic (blood-forming) stem cells. We combine this cell suspension with a preservative (DMSO) that protects the cells from damage during freezing. The "cryoprotected" cells are then transferred to a specially designed freezer bag.
Each cord blood unit is frozen using a controlled rate freezing. A record of the freezing curve is maintained on each unit.
Processing must be completed and cord blood units frozen within 36 hours of collection.
Frozen cord blood units are maintained in quarantine storage until infectious disease test results and bacterial culture test results are obtained.
After that cord blood units are released from quarantine and placed in permanent storage in liquid nitrogen.
Storage devices for cord blood units and associated samples have alarm systems that are continuously active. The storage freezers are connected to the Security Department of the Sheba Medical Center and under supervision during 24 hours.

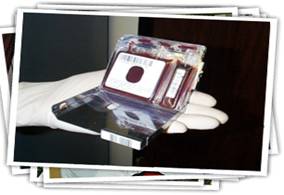
Shipping the cord blood unit for transplantation
After one or more cord blood units have been selected for transplantation, the Transplant Center may request shipment, on a specific date, scheduled to arrive before the patient begins conditioning to prepare for the transplant. For shipment, the unit is placed in a CryoShipper, a cylindrical container that stores liquid nitrogen within the shipper's honey-combed walls and maintains the inside temperature under minus 150°C for up to 7 days. A temperature monitor measures continuously and documents the temperature inside the shipper.